There are different types of diabetes and different treatment options for each type, so it’s difficult to generalize which supplements all people with diabetes should not take. That’s one of the reasons it is so important to talk to a health professional. All that said, here are five supplements you may want to reconsider if you have diabetes, as they may interfere with certain medications, disrupt blood sugar levels or cause unwanted side effects.
1. Chromium

Chromium is a mineral that is found in a number of foods, such as meat, vegetables, grains, fruits and nuts. A deficiency in chromium may cause high blood sugar; however, deficiency is very rare. If you have diabetes and take insulin or other oral medications aimed to reduce blood sugar, taking chromium may increase the risk of hypoglycemia (low blood sugar).
The American Diabetes Association cautions anyone with kidney disease against taking chromium because supplementation can worsen kidney disease. Chromium supplementation may also interfere with levothyroxine (a medication commonly used to treat hypothyroidism).
2. Bitter Melon
Bitter melon is an herbal supplement that has been studied for its use in reducing blood sugars in people with diabetes. Its components—charantin, vicine and polypeptide-p—are thought to have a similar structure to insulin (the hormone involved in blood sugar control).
In a systematic review and meta-analysis in Nature, researchers found that the data on bitter melon supplementation continues to remain inconsistent. Studies that have been done are short, and the doses of bitter melon used vary. More research is needed to determine long-term effects and safety. In addition, if you are prone to low blood sugar, bitter melon may increase your risk of low blood sugar and may not be appropriate for you.
3. Green Tea Extract
Drinking green tea has been shown to provide benefits for people with diabetes. For example, in a meta-analysis of 17 clinical trials published in The American Journal of Clinical Nutrition, researchers found that drinking green tea had favorable effects, such as decreased fasting glucose and hemoglobin A1C (three-month average of blood sugar). However, there is little research on the effectiveness of a green tea supplement outside of studies conducted on animals, and most studies have been very short in duration. Therefore, additional supplementation beyond drinking green tea is probably not necessary.
4. St John’s Wort
More research is needed on the use of St. John’s wort and diabetes, due its potential effects on diabetes medications, insulin sensitivity and insulin secretion. One small study in the British Journal of Clinical Pharmacology, which evaluated the use of St. John’s wort and metformin in 20 healthy male subjects, found that taking it in conjunction with metformin can increase insulin secretion and lower blood sugar after a glucose tolerance test. However, another very small study, including 10 healthy male subjects, found that there were no changes in insulin sensitivity when taking St. John’s wort alone. Instead, researchers noted less insulin secretion, which can increase blood sugar levels.
These very small studies had conflicting results and did not include diverse populations or people with diabetes or have a long enough duration to examine the long-term effects. Therefore, more studies are needed to explore the drug-herb interactions, as well as insulin secretion effects of St. John’s wort.
In addition, if you have diabetes and heart disease and are taking blood thinners, the ADA recommends avoiding St. John’s wort, as it can increase bleeding.
5. Vitamin E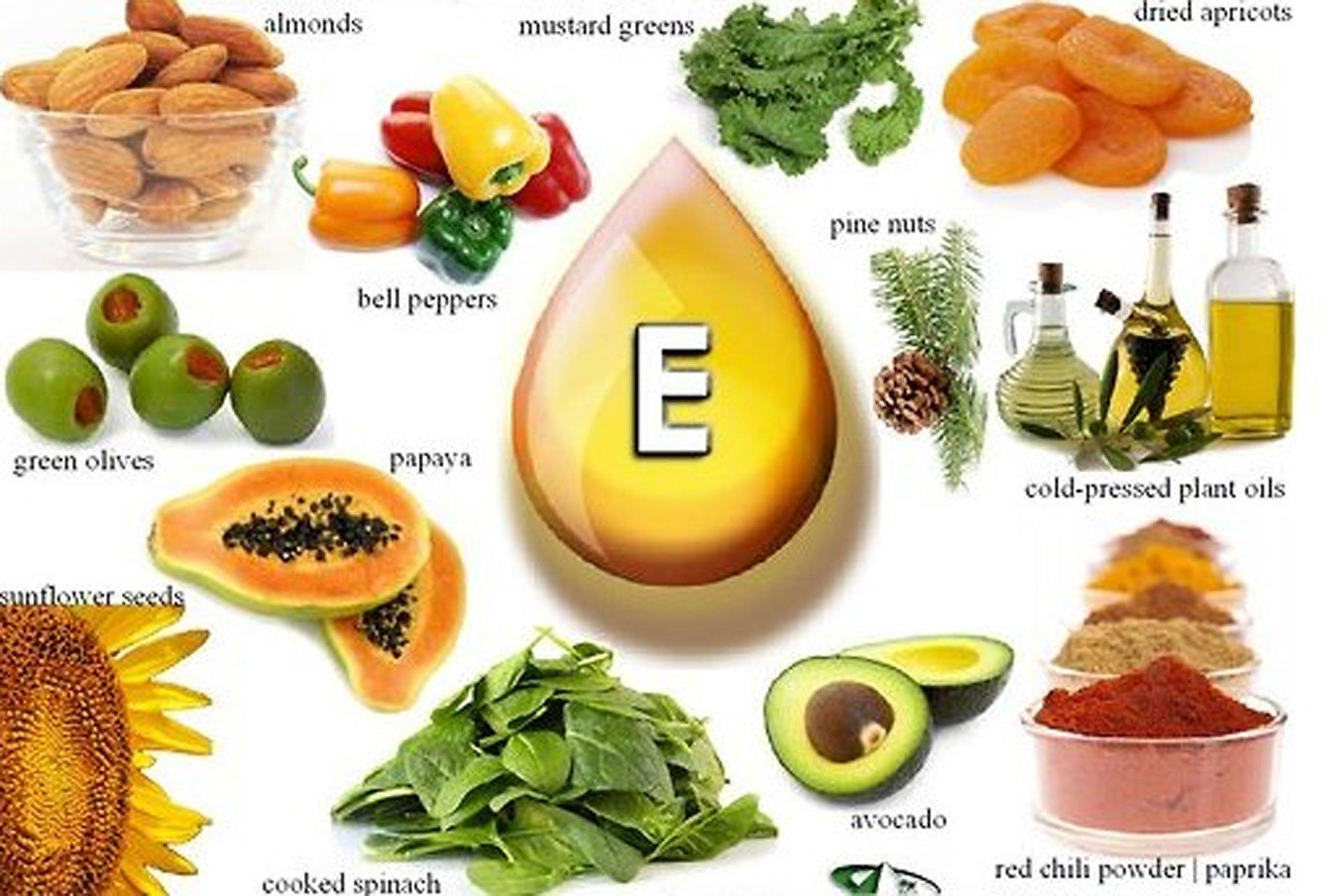
Vitamin E is a powerful antioxidant that can help combat oxidative stress, a precursor and contributor to type 2 diabetes. But, vitamin E can interact with blood thinners and increase the risk for bleeding by blocking the clotting effects of vitamin K. Therefore, unsupervised supplementation is not recommended if you have diabetes and are taking blood thinners.
Source: https://www.eatingwell.com